Genomic detectives are hot on the trail of deadly viruses
Matthias Pauthner, PhD, opened the internet browser on his laptop and there, snaking across the screen, was the heartbeat of a 4-year-old boy.
Pauthner sat at his small lab desk in La Jolla, California, surrounded by scientists working in white lab coats. The boy lay in a hospital bed in Sierra Leone, half a world away in West Africa, surrounded by nurses dressed head-to-toe in biosafety gear. The boy had Lassa fever, a disease that kills around 80 percent of the people who contract it. He was in the hot zone, fighting for his life.
A small white patch stuck to the boy’s chest connected the scientist in America and the young patient in Sierra Leone. Paired with a smartphone in the hospital where the boy was being cared for and where he was enrolled in a study of Lassa patients, the wireless heart monitor transmitted real time electrocardiogram readings of the boy’s heartbeat to a secure internet portal accessible to the doctors and research team in Sierra Leone and to Pauthner and his colleagues in California.
“We were able to record a continuous ECG reading of his heart for five consecutive days, something that isn’t even regularly done for patients in the United States,” said Pauthner, several months after the boy was admitted to the hospital. “His temperature when he was first admitted was really high, and his heart rhythm erratic. His heart stabilized the next day when his temperature came down. He lived, but it was touch and go initially.”

Pauthner is a postdoctoral researcher and part of a team of scientists at Scripps Research who study the life-and-death dance between humans and some of the world’s most dangerous viruses. Led by Kristian Andersen, PhD, an associate professor in the Department of Immunology and Microbiology at Scripps Research, the team has developed a unique system for studying pathogenic viruses, applying infectious disease genomics to track how viruses emerge and spread to cause large-scale outbreaks. They combine this deep profiling of viruses with medical data gathered from patients to look for clues to why some pathogens are more virulent and why some people are better able to survive infections.
Working with scientific collaborators around the globe, the team studies several dangerous viruses that have emerged in recent time. They include Lassa and Ebola viruses, highly lethal pathogens that cause viral hemorrhagic fevers, so named because the infection can cause blood vessels to rupture, resulting in severe internal and external bleeding.

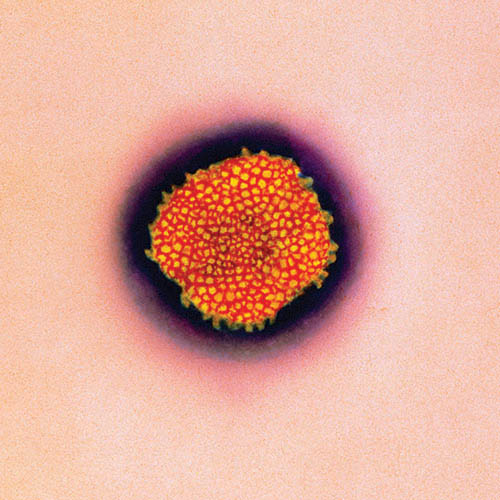
The Scripps Research team also focuses on Zika and West Nile, mosquito-borne viruses that were first identified in Africa but now plague other continents as well, including North America.
“We want to understand how these viruses travel so that we can improve early detection and predict how quickly a virus will spread,” says Andersen, who is also director of infectious disease genomics at Scripps Research Translational Institute. “Beyond that, our research aims to improve prevention, diagnosis and treatment of emerging viruses— whether they are known diseases or something we have yet to discover.”
Science in Sierra Leone
The Lassa fever research program in Sierra Leone is a case study in the promise and challenges of studying emerging viruses. Kenema district was a flashpoint of the civil war that engulfed Sierra Leone from 1991 to 2002. The region is rich in alluvial diamonds, which were used to finance the brutal rebel group, the Revolutionary United Front. The war-torn country was dramatized as the backdrop for the 2006 movie Blood Diamond, which starred Leonardo DiCaprio. As the country has recovered from the long conflict that killed around 50,000 people and devastated its infrastructure, including its health systems, it has contended with multiple outbreaks of endemic disease.
Andersen and his team are part of the Viral Hemorrhagic Fever Consortium, an international collaboration of researchers studying Lassa and Ebola with the intention of reducing the number of infections and deaths caused by the viruses. The consortium conducts research with local scientists and doctors at a hospital site in Kenema, the country’s second-largest city and capital of the Eastern Province, known for having the highest incidence of Lassa in the world. People who contract Lassa and come to Kenema for treatment are admitted to the Lassa ward at the Kenema Government Hospital. The Kenema ward was also used to treat Ebola patients during the 2013-2016 Ebola epidemic in West Africa that infected 28,000 people and killed more than 10,000.


Building relationships with Sierra Leone’s government and local research staff has been critical to studying the viruses. Mambu Momoh, a medical laboratory scientific officer of Sierra Leone’s Ministry of Health and Sanitation who works at the Kenema Government Hospital Viral Hemorrhagic Laboratory, says collaborating with Scripps Research scientists has been instrumental in expanding local expertise and capacity to respond to outbreaks. He worked on the front lines of the 2013-2016 Ebola epidemic and his team diagnosed the first case in Sierra Leone using diagnostics developed and deployed by Andersen and his colleagues.
“I have always enjoyed working alongside colleagues from the United States who are not only giving financial and logistic support to our site but also expertise and mentorship,” Momoh says. “It has been very inspirational for me, and I’ve gained much more experience in molecular biology science and gotten some high-tech training to enable us, the citizens, to carry out highly specialized scientific work in our lab.”
Members of the Scripps Research team travel to Sierra Leone to work with Momoh and the other local staff on research projects. Pauthner has been to Kenema twice for field work, most recently for a month in January 2019. Many of the roads were muddy from the heavy rains and the trip from the international airport in Freetown, the country’s capital, to the Eastern Province was a rugged five-hour drive in a 4-wheel drive truck. During the trip, he stayed at a compound in Kenema maintained by the Viral Hemorrhagic Fever Consortium as a base of operations for local research staff and visiting scientists.
One of Pauthner’s tasks was to teach the nurses at the hospital to apply the heart monitor patches to Lassa patients and sync the monitors to smartphones to transmit data via the internet. The patches are a pilot study that feeds data directly to researchers in the United States. He also worked in the hospital’s Viral Hemorrhagic Laboratory processing samples, which required donning a biosafety gown, double gloves, headcover, boots and goggles. The air conditioner for the lab is notoriously unreliable.
“Once, I was suited up and the air conditioner went out,” Pauthner says. “It got so hot I was soaked in sweat within minutes.”
Pauthner rode along on expeditions to villages in the Eastern Province where cases of Lassa had recently been reported. Lassa is transmitted from rodents to humans, typically when rats get into homes and infect food or when people eat the rodents. To prevent infections, local staff of Kenema Government Hospital travel to the villages to educate people on ways to avoid infections and unintentionally spreading viruses. Sierra Leone’s population is young, with about 42 percent under the age of 15, so the team piques their interest with popular African rap music and movies, then educates them on how to avoid infection.
The team also collected rats from the homes of people who caught Lassa to gather samples of viruses infecting the rodents. They collected blood samples from people in the villages who may have been recently exposed to infection. The blood samples are studied by the Center for Viral Systems Biology, a NIH-funded collaboration led by Andersen, that also includes Tulane University, University of California Los Angeles, MIT and Harvard Medical School. The center analyzes blood from survivors of past outbreaks of Lassa and Ebola to learn how they fought off the virus, merging computational analysis, machine learning and new technologies to discover how to minimize sickness and death in the future. One possible explanation for why some people fight off infections better than others is that they may produce special versions of immune system proteins, called human leukocyte antigens, that are particularly effective at recognizing infected cells. This would allow the immune system to more rapidly destroy infected cells, and hence clear the infection. Identifying and mimicking these highly effective variants could serve as the basis for developing new types of vaccines and antiviral drugs.
Troublesome family trees
In addition to deciphering what leads to different outcomes when humans become infected with a virus, the scientists also track how viruses spread. Similar to the way companies like Ancestry or 23andMe can trace a person’s ancestry by analyzing the DNA from a saliva sample, the Scripps Research team uses samples taken from various areas of Sierra Leone to create family histories of Lassa virus strains. Genomic similarity between different virus strains can be used to track how fast and far viruses spread as well as how quickly they evolve.
Creating viral family trees isn’t just an academic exercise. Deciphering what factors allow viruses to spread rapidly through and between host populations – whether rodents, insects or humans – is key to predicting and controlling future outbreaks. Some viruses move far more quickly than others. The global outbreak of swine flu in 2009, for example, took just six weeks to spread as widely as the typical seasonal flu travels in six months. First reported in Mexico, the flu rapidly spread around the globe, resulting in as many as 89 million cases and 18,000 deaths, according to the U.S. Centers for Disease Control and Prevention.
The rapid spread of Zika in the Americas is another case study of a virus taking a surprising turn and a severe human toll. Generally considered to be a mild disease, when Zika virus infects pregnant women it can cause serious birth defects in babies, including smaller heads and brain damage. First discovered in Africa in 1947, Zika was found in Brazil in September 2014. Using genomic analysis, Andersen’s team at Scripps Research determined that Zika circulated for more than a year and a half before being detected. From Brazil, a large outbreak spread throughout the Americas in 2015 and 2016, with 62 cases reported in travelers returning to the United States from affected areas in 2015, growing to more than 4,800 travel-related cases and 224 local mosquito-borne infections in the United States in 2016. The Scripps Research team also discovered that Zika entered Florida several times via travelers from the Caribbean before it was discovered. More recently, a genomics study of travel-associated Zika cases by Andersen’s team revealed an undiscovered outbreak in Cuba in 2017, underscoring the need for coordinated disease surveillance. This new field of “genomic epidemiology” will be critical to understanding and preventing future outbreaks.
Raphaëlle Klitting, PhD, another postdoctoral researcher on Andersen’s team, is attempting to explain why certain viral strains spread so aggressively. To do this, she uses skills honed as a graduate student at France’s Aix-Marseille University, where she studied yellow fever, an acute—and often fatal—viral disease transmitted by infected mosquitoes. Lassa virus is classified as a biosafety level 4 (BSL4) infectious agent, the most dangerous class, so working with the live virus in the United States requires an elaborate and expensive facility, including specially sealed rooms, pressurized protective suits and elaborate decontamination protocols. In the lab at Scripps Research, Klitting avoids the cost and hassle by working with what are called “surrogate systems,” safe noninfectious viruses modified to carry only a portion of the Lassa virus. Among other things, in recent experiments she has engineered surrogate viruses mounted with the molecular “key” Lassa uses to enter cells’ outer envelope. By swapping out different versions of the Lassa envelope, she tests their penetrating power.
“We want to know which variants are better at entering human cells versus rodent cells,” she says. “This could help us identify which strains are likely to jump from rats to humans or to spread from human to human. With this information, we can deploy countermeasures and stop that from happening. You could also imagine at the beginning of an outbreak analyzing the virus to predict how fast it could transmit and by what means it could spread, which could help public health officials respond more effectively.”
During her first visit to Kenema at the peak of the dry season in January 2019, Klitting came to appreciate that conducting research in a laboratory in Sierra Leone presents a different set of challenges than in a La Jolla laboratory.
To freeze safe, deactivated samples to ship outside Sierra Leone, the team needed liquid nitrogen, but the liquid nitrogen generator was struggling because the air conditioner couldn’t cool the room enough. Klitting and her colleagues were coaxing the machine to eke out just enough liquid nitrogen when their generator ran out of fuel and they had to wait days for a money wire to buy more.
“Doing field work really made me a better scientist,” she says. “You have to structure your research to work with the conditions you’re given. And it’s where you see what’s happening in real life, where the virus is spreading.”
She was also impressed with the bravery and skill of the hospital’s medical staff, many of who put themselves at risk caring for patients during past Lassa and Ebola outbreaks. Tragically, during the 2013-2016 Ebola epidemic, several of the hospital staff became infected and died from caring for patients.
“It’s remarkable how they stay motivated,” she says. “Some people are just heroes.”